A team of researchers at the RCSI Department of Obstetrics and Gynaecology at the Rotunda Hospital, Dublin will today launch three research studies examining the experiences and impact of diabetes in women, ahead of World Diabetes Day 2019.
The three studies have been awarded total funding in the region of €1.1 million by the Health Research Board (HRB) and the European Commission.
The studies will look at the impact of diabetes in pregnant women and comprise a clinical trial, a research study, and a creative project.
The IRELAnD Trial will examine the role that aspirin plays in improving the health of pregnant women with diabetes. This is the first study to examine the impact of low-dose aspirin for the prevention of preeclampsia (high blood pressure during pregnancy) in women with diabetes. The trial will recruit over 550 women across seven maternity hospitals in Ireland over the course of the next three years.
Professor Fionnuala Breathnach, Consultant Obstetrician and Gynaecologist with RCSI and The Rotunda Hospital, said:
“Previous studies have shown that low-dose aspirin has an impact on reducing the risk of high blood pressure and other complications in some pregnancies. Through this study, we want to understand whether this benefit could be applied to pregnant women with diabetes. Preeclampsia is a high-risk complication that affects 2-3% pregnant women in Ireland each year, and rises to 5-7% in first time pregnancies, and can be particularly problematic when the woman has a long-standing history of diabetes. These pregnancies can be quite complicated, and any opportunity that we have to explore ways of reducing risk is an opportunity of a lifetime for this research team.”
The second study undertaken by RCSI is with BigMedilytics, an international collaboration between partners from academia and industry across Europe. It will assess whether self-monitoring of blood sugar levels, using glucometers connected to a mobile app, and then using App- assistance for management of gestational diabetes (GDM)by the woman and by the clinical team may reduce the number of required hospital visits for women.
Currently, patients with GDM need to attend specialised diabetic clinics where obstetricians, endocrinologists, and dieticians can review them. These visits often involve long waiting times and consume patient and hospital resources, while only providing a snapshot of diabetes control. Through the ‘GDMapp’ app, the patient has a much more straightforward way of documenting their blood sugar results and sharing them with their clinical team.
Dr Elizabeth Tully, Programme Manager of the HRB Mother and Baby Clinical Trial Network, said:
“Working with BigMedilytics, we hope to understand how self-monitoring solutions, like smart glucometers, can be used to reduce the amount of hospital appointments and expert management required for women with gestational diabetes. If this proves possible, the results of this study will have a positive impact on women, who may need to attend fewer specialised diabetes clinics and hospitals, which are already stretched well beyond capacity.”
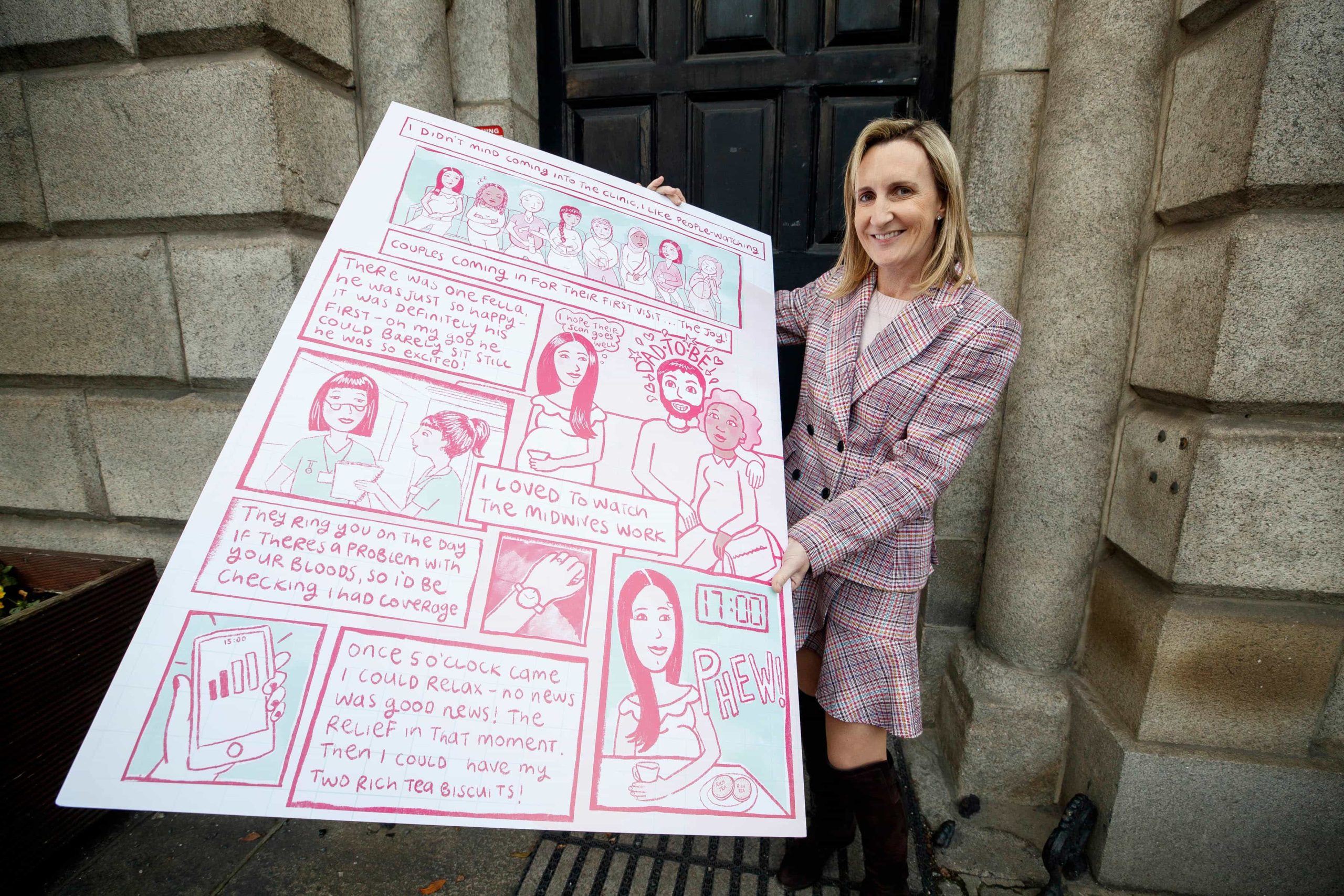
The third project aims to share the story of diabetes in pregnancy in Ireland. In an online comic, the study will follow the lives of women with diabetes during their pregnancies.
With insights drawn from interviews with real women and illustrated by artist Fiona Carey, The Breakfast Club comic shares the full scope of these women’s experiences with diabetes during pregnancy. From learning to manage a new diet to getting to grips with using insulin, the study will illustrate their hopes, frustrations, tragedies and joys. The comics will be available to view and download on breakfastclubcomic.ie
Fiona Carey, artist of The Breakfast Club, said: “Pregnancy is an exciting, overwhelming, and challenging time for expecting mothers. For pregnant women with diabetes, it can be even more difficult, even isolating. Through The Breakfast Club project, we hope to demystify the condition and to translate these women’s hopes, frustrations, tragedies, and joys into art in the hope that it will provide clarity and support to pregnant women with diabetes across Ireland and the world.”
Gestational diabetes develops in women during pregnancy because the mother’s body becomes resistant to the effects of insulin. Levels of sugar in the woman’s bloodstart to rise. High blood sugar levels in the mother’s body are passed through the placenta to the developing baby. This can cause significant health problems for the baby if left untreated.
Gestational diabetes usually begins in the second half of pregnancy and goes away after the baby is born.
Gestational diabetes affects 5-10% of Irish women.
Pre-gestational diabetes occurs when women have diabetes (type 1 or type 2) before becoming pregnant. Women with pre-existing diabetes are at a higher risk of developing pregnancy complications, from high blood pressure related complications, to poorly functioning placenta. Babies of diabetic pregnancies may have an increased risk of diabetes in later life.
Moreover, the incidence of pre-gestational (Type 1 and Type 2) diabetes is increasing. In 2014, 5.1% of women in Ireland had diabetes (The Lancet, 2016 https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)00618-8/fulltext#seccestitle160).
The incidence of type 2 diabetes mellitus is increasing in younger people, with many women of childbearing age developing type 2 diabetes (HSE guidelines, 2010).
This is why an optimal management and care of diabetes before and during pregnancy is of great importance, for the mother, the baby, and the whole society.
The total number of people living with diabetes in Ireland is estimated to be 225,840 (diabetes Ireland)