All women are encouraged to attend the general nutrition class (live) presented by our dietitians. You can discuss with your midwife during your booking visit, or by ringing outpatient reception desk to book yourself in. If you cannot attend, a full recording on the class can be found here.
Staying healthy during pregnancy
The Rotunda Hospital Dublin
HEALTHY EATING DURING PREGNANCY
Healthy eating is important for everyone, but it is particularly important during pregnancy as your baby is growing and developing. During pregnancy, you can also help to lower your baby’s risk of disease later in life and keep yourself well and healthy by eating enough of the right foods.
1.1 What is a healthy diet?
Your diet should include a wide variety of foods, low in fat, sugar and salt, and rich in whole grains, fruit, vegetables and calcium. The food pyramid is a guide to getting a good balance of each food group in your diet.
- Include 3 main meals and 2-3 healthy snacks each day
- Aim to have half of your plate as fruit or vegetables at each main meal
- In the second half of pregnancy, aim to include an extra serving of protein-rich foods (e.g. lean meat, chicken, fish, eggs, beans and nuts) each day
- Choose wholegrain breads, cereals, rice and pasta for extra fibre and nutrients
- If you are expecting twins (or more) or if you are a teenager, you should aim to have 5 servings of dairy (or calcium-rich alternatives) every day
- Only have processed meats, fast food, sugar, cakes, biscuits and sweet desserts occasionally (not daily)
1.2 Important nutrients for pregnancy
These nutrients are particularly important during pregnancy:
-
Folic acid (folate)
-
Iron and vitamin C
-
Calcium and vitamin D
-
Omega-3 fatty acids
-
Iodine
1. Folic acid
Folic acid is an essential vitamin to help your baby’s spine form properly during early pregnancy. Folic acid helps to prevent spina bifida and other neural tube defects in your baby. The baby’s spine develops very early in pregnancy, even before you may realise you are pregnant, so it is important to start taking folic acid before you become pregnant – ideally at least three months before each pregnancy. If you didn’t take folic acid before your pregnancy, you should start to take 400 micrograms (400µg) straight away and continue to take it for the entire pregnancy. You can buy folic acid supplements over the counter from your pharmacist. You should also include folate-rich foods in your diet every day during pregnancy, such as green leafy vegetables, fortified breakfast cereals, beans and citrus fruits.
Note: If you have a body mass index (BMI) above 30kg/m2, have diabetes or are taking medication for a condition such as epilepsy, it is important to talk to your doctor as you may need to take a higher amount of folic acid. Tell your doctor or midwife about all medicines and supplements you are taking to be sure they are safe for pregnant women.
2. Iron and vitamin C
Iron is essential to make the extra blood that you and your baby need during pregnancy. This is important to move oxygen around your body and to help your baby’s brain to develop. If you don’t have enough iron in your diet, you can get anaemia (low levels of iron in your blood) which may cause you to feel tired, short of breath and have no energy. Your baby could also be anaemic at birth. You can improve your levels of iron by eating foods high in iron every day.
You should include one serving of these a few times per week:
- beef, lamb or pork
- chicken or turkey
- salmon, sardines, trout and mackerel (one to two times a week)
- tuna – up to 280 grams (drained) a week
You should include one or more of these good iron sources with each meal:
- eggs
- wholegrain bread
- iron fortified breakfast cereals
- dark green leafy vegetables: cabbage, brussels sprouts, spinach, kale, broccoli
- beans: kidney, chick peas, baked beans, peas, or pulses like lentils
- dried fruit: apricots, raisins, sultanas, prunes
Vitamin C helps to absorb the iron in vegetables. Take good vitamin C sources daily:
- oranges, orange juice, grapefruit, lemons, limes, strawberries, melon, kiwi or vitamin C fortified fruit juice
- green, red, yellow peppers or fresh tomatoes
If you are taking an iron supplement, wait 30 to 60 minutes after a meal before taking it, as some foods can reduce the amount of iron you can absorb. It can also help to take your supplement with some vitamin C.
Iron supplements can stop some blood pressure medications or thyroid medications from working properly. Take your iron tablet and any other medications you have been prescribed at least two hours apart.
3. Calcium and vitamin D
Calcium is an important mineral for healthy bones and teeth and for regulating blood pressure. Foods that have a lot of calcium are milk, cheese, yoghurt, fortified soya milks and fortified orange juice. Take three portions of these foods every day. If you are having twins or more, or if you are a teenager, take 5 portions daily.
One portion of calcium rich food is:
- 200 ml fortified cow’s milk or calcium-fortified milk alternative
- 30 g cheese
- 125 g yoghurt
- 45 g tinned sardines (eaten with the small, soft bones)
You also need vitamin D to absorb the calcium from your diet. Vitamin D may also help support your immune system and general health. All pregnant women should take a supplement of10 µg (400 IU) Vitamin D daily and choose foods rich in vitamin D (salmon, mackerel, sardines, milk, spreads with vitamin D).
4. Omega-3 fatty acids
Omega-3 fatty acids, DHA and EPA, are important for your heart and for baby’s brain, eyes and nervous system development. Aim to eat salmon, mackerel, sardines, trout or herring once weekly. If you do not eat fish, take a vitamin and mineral supplement made for pregnancy that contains iodine and omega-3s.
Some types of fish contain too much mercury or other toxins that may be harmful to your baby. Do not eat shark, marlin, ray or swordfish. Only eat one tuna steak or two cans (140 g drained weight) of tuna in a week. This also applies if you are breastfeeding.
5. Iodine
Iodine is important for your baby’s brain development. Fish and dairy products are rich sources of iodine and should be included in your diet.
Vegetarian and vegan
If you are vegetarian and your diet is varied and balanced, you will get enough nutrients for you and your baby during pregnancy. However, it can be hard to get enough iron, iodine, vitamin D and vitamin B12 from a vegetarian or vegan diet. Take a complete vitamin and mineral supplement that is made for pregnancy to ensure you are meeting your needs for these essential vitamins and minerals.
Other special diets
If you follow another type of restricted diet because of food intolerance (for example, coeliac disease) or for religious reasons, talk to your doctor or midwife. The dietitian can advise you on how to make sure you are getting all the nutrients you need for yourself and your baby.
1.3 Sample healthy menu for pregnancy
1.4 Foods to avoid during pregnancy
Certain foods should be avoided during your pregnancy because they can have bacteria in them, too much vitamin A or other toxins that may harm you or your baby.
Don’t eat:
- Raw/undercooked eggs, homemade mayonnaise or mousse made with raw eggs
- Unpasteurised or mould-ripened and blue-veined cheese such as Brie, Camembert or Stilton
- Unpasteurised milk products or juices
- Raw or undercooked meat, poultry or fish and pâté
- Do not take cod liver oil supplements or a standard multivitamin as they contain large amounts of vitamin A which may cause birth defects in babies
- Avoid herbal supplements and tell your doctor, midwife or dietitian about any supplements you decide to take
- Avoid alcohol (wine, beer or spirits). No amount of alcohol is considered safe in pregnancy
- Do not take protein supplements
Caffeine in large amounts may be harmful. Caffeine is found naturally in coffee and tea and cola drinks. It is also added to other soft drinks, ‘energy’ drinks and some cold and flu remedies. You should only drink a total of 200mg per day e.g. two cups of coffee, three to four cups of tea and two cola drinks a day. Try drinking decaffeinated tea and coffee or water instead. Only take cold remedies if advised by your doctor.
Pregnant women do not need to avoid any foods such as nuts, peanuts, eggs or milk products to prevent baby from forming an allergy. It is best to eat a varied diet but avoid foods if you have an allergy to them yourself.
1.5 General good food hygiene practices
- Wash your hands before and after handling any food
- Thoroughly wash all fruit and vegetables before eating them
- Cook raw meat and poultry thoroughly
- Make sure that you properly reheat ready-to-eat poultry and cooked chilled meals and they are piping hot before you eat them
- Use a separate chopping board for raw meat
- Keep cooked food and raw food away from each other
- Make sure that your fridge is below 5°C
- Put chilled food in the fridge straight away and eat it as soon as possible
- Throw out food that is gone past the ‘use by’ or the ‘best before’ date
COMMON PROBLEMS DURING PREGNANCY
The hormones of pregnancy can change the way your digestive system works. These are the most common problems along with some information on what you can change in your diet to help you cope:
2.1 Morning sickness
This is the nausea and often vomiting that affects many women in the first 12 to 15 weeks of pregnancy. Many women can cope with morning sickness by snacking little and often on bland, easy-to-digest foods such as plain toast, crackers, cereal or plain biscuits. Be aware of cravings and eat whatever you feel you can. When symptoms improve, increase the variety of foods as tolerated. Aim for a varied diet and drink plenty of fluids. Talk to your doctor if you are unable to hold down any food or fluids or are losing weight. If you are unable to tolerate a multivitamin as a tablet, try a liquid multivitamin as it may be better tolerated.
2.2 Heartburn
This is the burning or acid feeling in the chest or throat that affects many women, usually later in the pregnancy. Eat small, frequent meals and avoid eating meals before bed time. Stay upright for at least one hour after each meal and eat slowly at meal times. Avoid very spicy and fried or oily foods, fizzy drinks, caffeine and chocolate if they cause a problem for you. Low-fat milk may help soothe the burn. Raise the head of your bed or use extra pillows and wear loose, comfortable clothes to reduce pressure on your tummy.
2.3 Constipation
This is infrequent bowel motions or the presence of hard, difficult to pass stools. It can be relieved with high fibre foods (fruit, vegetables and wholegrains), prune juice, plenty of fluids and regular exercise. Eat foods such as wholemeal bread, beans, pulses, fruit and vegetables, wholemeal pasta and brown rice instead of the white, processed types. Drink a minimum of 2 litres of water every day. Try to get 30 to 45 minutes of gentle exercise daily such as walking or swimming. Do not take laxatives unless they are prescribed by your doctor.
It is important not to strain when you empty your bladder and bowels to protect your pelvic floor muscles. The best position to sit on the toilet is pictured below.

- Always sit on the toilet seat. Do not hover above it, even when just emptying your bladder
- Use a foot stool or raise your heels so that your knees are higher than your hips
- Lean forward, with your feet apart and your elbows on your knees
- Breathe in and let your tummy gently swell out
- Breathe out as you push down towards your back passage
- Your tummy should stay braced out and don’t allow your tummy to suck back in again
- Repeat as necessary
- Allow yourself time, do not rush
WEIGHT GAIN DURING PREGNANCY
A healthy rate of weight gain throughout pregnancy is important for the healthy growth and development of your baby. It also helps to lower your baby’s risk of disease later in life and keeps you well.
There are a number of things that contribute to weight gain during pregnancy, including the weight of your baby, placenta, amniotic fluid, along with changes in your own body to support the pregnancy.
Women should gain very little weight 0.5 – 2 kg (1 – 4 lb) in the first trimester, with most weight gain occurring in the second and third trimester. At your first antenatal visit the midwife will record your weight and height to calculate your Body Mass Index (BMI). The table below will guide you on how much weight you should gain depending on your BMI category.
| Recommended total weight gain and average weekly weight gain in 2nd & 3rd trimester | ||||
| Kilograms | Stones and pounds | |||
| BMI category | Total weight gain | Rate of weight gain (2nd & 3rd trimester) | Total weight gain | Rate of weight gain (2nd & 3rd trimester) |
| Underweight
(less than 18.5) |
12.7 – 18.2 kg | 0.5 kg per week | 2 – 2 st 12 lb | 1 – 1 ½ lb |
| Normal weight
(18.5 – 24.9) |
11.4 – 15.9 kg | 0.4 kg per week | 1st 11 lb – 2st 7 lb | 1 lb |
| Overweight
(25 – 29.9) |
6.8 – 11.4 kg | 0.3 kg per week | 1 st – 1 st 11 lb | ½ – 1lb |
| Obese
(more than 30) |
5.0 – 9.0 kg | 0.2 kg per week | 11 lb – 1 st 6 lb | ½ lb |
3.1 Underweight and multiple babies
If you are underweight (BMI less than 18.5) or are carrying more than one baby, you may be at risk of premature delivery or having a baby with low birth weight. It is important to gain enough weight to support your baby’s growth as well as your own health.
3.2 Overweight
Being overweight or putting on too much weight during pregnancy can affect your health in a negative way and can increase the risk of complications to both you and your baby.
These include:
- Thrombosis / blood clot
- High blood pressure
- Gestational diabetes
- Pre-eclampsia
- Difficulty using vitamin D stores
Weight loss is not recommended during pregnancy. If you are overweight or are gaining too much weight during pregnancy, we can give you extra help and support during pregnancy to minimise the risk of complications for you and your baby. If you are concerned about your weight, talk to your midwife or doctor. They can arrange an appointment for you to see the dietitian. The dietitian will focus on minimising weight gain during your pregnancy and on healthy eating.
Eating a healthy diet can help to reduce the risks in this pregnancy and in future pregnancies.
- Eat three meals and some snacks spaced throughout the day
- Limit fatty or fried foods and takeaways
- Avoid added sugars and sugary foods
- Do not skip meals. You may find yourself eating too much at the next meal because you are overly hungry
- Stay active every day by taking time for exercise such as walking, swimming or pregnancy yoga
Remember that even if you are overweight, weight loss is NOT recommended during pregnancy. The best time to lose weight is before or after your pregnancy.
WOUND HEALING
Healthy eating after birth will contribute to faster and effective wound healing. It is important to continue choosing a wide variety of food. In addition, extra protein, vitamins and minerals (especially vitamin C and iron) will improve your wound healing.
Aim to include some protein at each meal and include some protein-rich snacks throughout the day. These include:
- Meat, chicken, turkey and fish
- Eggs
- Cheese, yoghurts and milk
- Beans, peas or pulses
Vitamin C is also important for wound healing. Aim for at least 5 servings of fruit and vegetables per day with at least 2 servings from vitamin C rich foods, such as:
- Oranges, orange juice, grapefruit, lemons, limes, strawberries, melon, kiwi or Vitamin C fortified fruit juice
- Green, red, yellow peppers or fresh tomatoes
Tips to promote wound healing:
- Eat more often if you can’t eat a lot. Aim for 6 smaller meals rather than 3 big meals a day, which may be too filling
- Have your favourite foods in the cupboard or fridge
- Keep ready-to-eat meals and snacks handy for times when you don’t feel like preparing food (e.g. frozen meals, yoghurt, nuts, cheese, biscuits and dips)
- Drink fluids that provide energy such as milk, juice, cordial or soft drink, instead of tea, coffee or water
YOUR EMOTIONAL AND MENTAL WELLBEING
Your emotional and mental wellbeing are also key to your healthy pregnancy. From the moment you suspect or confirm that you are pregnant, things begin to change. Finding out you are pregnant is usually a very emotional experience – you are either delighted, terrified, or somewhere in between.
What surprises many women and their partners is the ongoing emotional changes that they feel during their pregnancy. This is perfectly normal, but understanding what to expect and why, will help both you and your partner get the most enjoyment out of this amazing experience. Your feelings change – about yourself, your baby, your relationships and your future. You begin to think about the realities of being a mother and how you will adapt to this new role. Many women think more about their own childhood and their relationship with their own mother during pregnancy.
If this is your first pregnancy you may feel a little anxious about being a good parent, and about caring for your baby. This is perfectly normal – most women worry about not being able to cope with the day-to-day baby care. Having a good support network in place like your partner and family before the birth will help you feel more confident that you can do it, so make sure you discuss your fears and worries with them. Try and learn as much as you can about caring for a newborn baby, and speak to other mothers that you know. Having this knowledge will make you feel better prepared when your baby is born.
There will be big changes in your hormone levels during pregnancy. It is common to have mood swings and it is not something you have much control over. Nearly all pregnant women have emotional ups and downs. You can have times of feeling unsure and panicky, having extreme reactions to minor things and crying. Getting used to the changes in pregnancy is not always easy. Changes in your hormone levels also mean you have physical symptoms like feeling sick and tiredness, so remember to get plenty of rest and continue to do what you enjoy doing. Talking about your feelings and your concerns to your partner, or to somebody close to you, will help to put things in perspective and help you to cope.
It is normal for couples, and especially the mother, to worry about the health of their baby. What if there is something wrong? Will he or she be normal? It is helpful to know that many other pregnant women have worries, anxieties and fears like yours – about pregnancy, labour and looking after a new baby. Although it is normal to have some worries while you are pregnant and to feel a bit down from time to time, it is more serious if you are feeling low or depressed a lot of the time. Talk about your concerns with your GP, midwife or obstetrician. The parent education classes will help to answer some of your concerns and you will have an opportunity to talk with other women who are around the same stage in pregnancy as you.
5.1 Depression
While most women feel that pregnancy and new motherhood is a happy time, another group of women find that they cannot feel happy at all. About one in five women have some level of depression in pregnancy – they worry, lose confidence, don’t sleep well and become exhausted. They think they are unlovable and unattractive, their relationships go wrong and they can feel numb, trapped and dull with little interest. They may feel irritable and angry. They may have a continuous bad mood.
When you feel depressed, it may seem that no one cares or that nothing else matters. We don’t usually know the reason for having a low mood or depression in pregnancy. If you have had depression in the past then there is a risk it will happen again when you are pregnant and afterwards. There are many ways to treat depression in pregnancy. You can manage mild to moderate depression by having a well-balanced approach to life. Having a good diet and exercising will help you to stay well and overcome your low mood and depression. Some women need anti-depressant medication to control the difficult effects of their depression. If you are taking antidepressant medication and you unexpectedly get pregnant, talk to your GP before you stop taking your medication.
A bad day is normal. A bad week is not. Talking to someone you trust is helpful. Accepting help early on means you could have a quicker recovery. If you are anxious about your pregnancy or the birth of your baby or had a previous difficult birth, then talking with your GP or midwife will help. If you feel anxiety or panic attacks are affecting your ability to do your normal activities then seek help early from either your GP or support midwife.
The Rotunda offers women a supportive perinatal mental health service. Talking helps women to develop a sense of perspective about the situation and allows them to think about what steps they can take to get back a sense of control in their life. We have dedicated midwives who are happy to offer support and information to any woman who needs it during their pregnancy and after the baby’s birth.
To make an appointment with the mental health support midwife, telephone 01 817 2541 or 087 671 4086. Excellent information on mental health in pregnancy and postnatal mental health is available on the Royal College of Psychiatrists website: www.rcpsych.ac.uk
Although it might sound like your pregnancy is going to be nothing but a long string of emotional crises, this is not the case for most women. You will have various ups and downs, but you will usually be able to manage these, especially if you have a supportive and involved partner. Remember that most pregnant women experience all the emotions you are going through. They are perfectly normal and you shouldn’t allow yourself to get stressed by them. Pregnancy is a wonderful experience, so don’t allow normal emotional changes to ruin that experience for you!
Finally, remember that one of the main tasks for you during the nine months of your pregnancy is to mentally prepare yourself for motherhood. To successfully prepare yourself for becoming a mother you need to be completely honest and open about these feelings.
Making sure you are safe
Research shows that some women are at greater risk of violence from their partner when they are pregnant. This can be physical, emotional, verbal or sexual abuse. If you are worried about this, you can speak in confidence to the hospital social worker on 01 817 1722 or contact the Women’s Aid National Helpline at 1800 341 900, which is open 24 hours a day, 7 days a week.
EXERCISE IN PREGNANCY
To stay healthy and well, pregnant women should take regular exercise. As well as being good for your heart, breathing and muscle tone, exercise helps reduce stress levels, improve sleep and can prevent you from getting pain around the pelvis and low back areas. Exercise can also help you manage your blood sugars, gestational diabetes and prevent you from putting on too much weight.
Exercising regularly, will help you get ready for labour and after your baby’s birth, will help you get back into shape.
If you are healthy and well, and have no problems with your health before or during your pregnancy, you should do 30 minutes of moderate exercise at least five days a week. You can divide this up into two 15 minute sessions a day if it is easier for you.
If you have medical or pregnancy problems, or are worried about your health, you should talk to your doctor, midwife or physiotherapist before exercising.
Helpful hints
- Moderate exercise means that you are doing something that is quite hard but that you can still carry on a conversation. This is known as the ‘talk test’.
- If you didn’t exercise regularly before pregnancy, start by doing some gentle exercise and build up to moderate exercise.
- Pregnancy hormones can soften your ligaments; therefore it is important to protect your joints during exercise. We recommend that you do low impact exercises and avoid exercises with a risk of falling. Walking is a great free way to exercise.
- Start with a gentle warm up and finish with a cool down.
- Drink plenty of water and avoid becoming too warm during exercising.
- Listen to your body and stop when you feel tired or if it hurts. Never exercise if you are feeling unwell.
- Wear good supportive shoes and a supportive bra/underwear when exercising.
- If you go to exercise classes, make sure that your teacher knows that you are pregnant.
- Swimming is a great way to exercise during pregnancy and the water will support your extra pregnancy weight. If you have pain around the front of your pelvis, it is best to avoid the breast stroke as the movements might make the pain worse.
- From the 16th week of your pregnancy avoid lying flat on your back to do exercises because you might feel faint or short of breath.
- Always avoid doing sit-ups. It can stretch your tummy muscles further and lead to back pain.
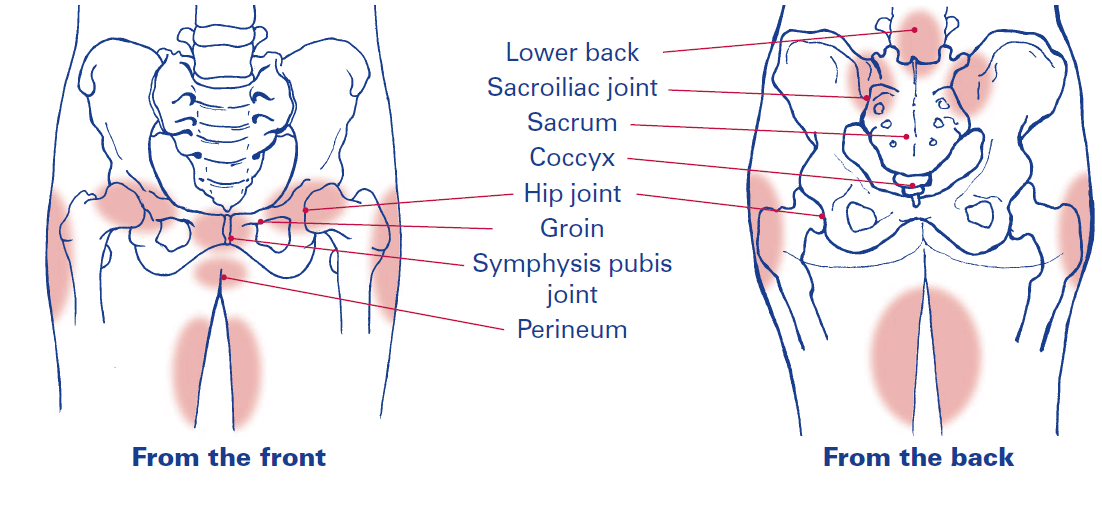
6.1 Pelvic Girdle Pain (PGP)
Pelvic girdle pain describes pain in any of the three pelvic joints. It is common but not normal and can affect 1 in 5 women during pregnancy. There are many causes which include:
- Uneven movement of the pelvic joints
- Changes in the activity of the tummy, pelvic girdle, hip and /or pelvic floor muscles affecting the stability of the pelvic girdle
- Previous injury to the pelvis
- Hormonal changes that occur during pregnancy
- The position of the baby can cause symptoms related to pelvic girdle pain in some women
You may experience:
- Difficulty walking
- Difficulty with activities requiring standing on one leg e.g. climbing the stairs, dressing or getting in or out of the bath
- Pain and/or difficulty moving your legs apart e.g. getting in and out of the car
- Clicking or grinding in the pelvic area – you may hear or feel this
- Limited or painful hip movements e.g. turning over in bed
- Difficulty lying in some positions e.g. on your back or side
- Pain during normal daily activities
- Pain and difficulty during sexual intercourse
With pelvic girdle pain the degree of discomfort you are feeling may vary from being intermittent and irritating to being very wearing and upsetting.
Management of pelvic girdle pain during pregnancy:
- Your doctor or midwife may refer you to a physiotherapist. You will be given an appointment for our special class which provides advice, exercises and information to help you manage your pain and daily activities.
- Your physiotherapist may then arrange a one to one appointment and do an assessment of your spine and pelvis and she can recommend a range of treatment options.
- Manual therapy, which is a ‘hands on’ treatment may be required to ensure your spinal, pelvic and hip joints are functioning normally.
- A pelvic belt may be given to provide added stability, if appropriate.
- Crutches may be used if pain is severe on weight bearing.
Things you can do to help reduce the pain:
- Be as active as possible within pain limits and avoid activities that make the pain worse
- Rest when you can – you may need to rest and sit down more often
- Ask for and accept help with household chores from your partner, family and friends
- Pull in your tummy muscles (as if you are hugging your baby) before going from sitting to standing and from standing to sitting
- Go up stairs one leg at a time with the pain free leg first. You may need to try going upstairs backwards or on your bottom
- If getting in and out of the car is painful, sit on the seat first and try to keep your knees together or step them (lift one up and then the other) into the car; a plastic carrier bag on the seat may help you to swivel
- Sit down to get dressed and undressed and wear flat supportive shoes
- Sleep in a comfortable position e.g. lie on your side with a pillow between your legs and feet
- When turning in bed, it can help to keep both knees together and try to turn under rather than over on your back in one smooth movement


- Roll in and out of bed keeping your knees together
- Maintain a good posture by standing tall and keep a gentle curve in your lower back
- If using crutches have a small rucksack to carry things in
- Have a toddler at waist height when changing their nappy and kneel beside the bath when bathing children
AVOID activities which make the pain worse:
- Avoid or reduce unnecessary weight bearing activities, for example, shopping, lifting or activities on one side, such as carrying a toddler on one hip
- Lifting or pushing heavy objects or carrying anything in only one hand
- Plan your day – avoid unnecessary trips up and down the stairs
- Standing on one leg, crossing your legs or sitting twisted
- Sitting or standing for long periods
Pelvic floor muscles
These are very important muscles as they control the bladder and bowel. During pregnancy they become weakened due to pregnancy hormones and the extra weight of your baby. It is important for all women to strengthen their pelvic floor muscles during pregnancy, whether they plan to have a vaginal delivery or caesarean section.
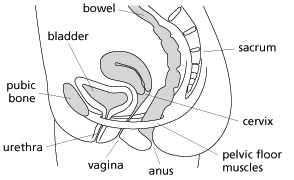
Exercises for your pelvic floor muscles
To begin with, lie on your back with your knees bent and your feet hip width apart or over on your side.
Long holds
-
- Breathe in and let your tummy gently expand and your pelvic floor relax downwards. As you breathe out, squeeze and lift your pelvic floor. Starting at the back passage, squeeze as if you are trying to stop yourself passing wind and then urine. You may feel your lower tummy tighten gently.
- Hold for 3 seconds; keep your upper tummy, buttocks and thigh muscles relaxed and breathe normally.
- Relax completely for 3 seconds. Repeat this exercise 5 times. Repeat 3 times a day.
- As your pelvic floor muscles get stronger, practice in sitting and standing.
- Gradually increase the length of time and number of repetitions until you can do a 10 second hold 10 times. Always stop exercising when the muscle gets tired.
If you feel more pain when you do this exercise, you should stop and make an appointment to see one of our physiotherapists to review your pelvic floor muscles.
Quick holds
-
- Quickly tighten the pelvic floor muscles and hold for a second before letting go fully. Breathe normally as you do this.
- Repeat 5 times in a row. Repeat 3 times a day.
- Gradually increase your repetitions until you can do 20 quick squeezes in a row; it may take a few months to be able to do this.
The knack
- Quickly squeeze and hold your pelvic floor muscles BEFORE coughing, sneezing, laughing and when lifting your baby. This will give you more control of your bladder and will help to keep your muscles strong.
To be effective you need to do your pelvic floor muscle training 3 times a day. An app, for example Squeezy from the NHS may help you to remember to do them.
Pelvic floor muscle exercises – information
Knowing how to do your pelvic floor muscle exercises is really important and can help you prevent or stop urine from leaking.
The physiotherapists in the Rotunda Hospital have made five videos on learning about pelvic floor muscles, doing your pelvic floor muscle exercises, leaking urine and doing exercises after you have your baby. The videos can be accessed on our website: www.rotunda.ie. Each video is just 3-6 minutes long.
If you experience incontinence of urine during your pregnancy, please tell your midwife or doctor and they can refer you to a physiotherapist.
6.2 Yoga for pregnancy and birth
The word ’yoga’ means ’union’ in Sanskrit, the classical Indian language. The practice of yoga is a coming together of the mind, body and spirit. Although yoga in pregnancy follows the same principles as all yoga, it is quite different from regular yoga because it is designed with the specific needs of the pregnant woman in mind. Because of this, yoga in pregnancy is always safe and gentle.
The benefits of yoga during pregnancy are:
- Yoga exercises gently work on the reproductive organs and pelvis and may help you have a smooth pregnancy and a relatively easy birth;
- Practicing yoga might help to develop self-awareness and harmony between body and mind;
- As a therapeutic tool, yoga meditation might help you resolve your fears and worries which are so common during pregnancy.
- Yoga improves deep breathing, which allows more oxygen to enter the bloodstream;
- Yoga promotes good posture, easing upper and lower back pain;
- Regular practice will improve muscle tone and strength, with improved control of balance and co-ordination;
- Yoga can help to increase the circulation of blood and lymphatic drainage which reduces the risk of swelling, varicose veins and piles (haemorrhoids);
- Yoga can help to increase stamina and endurance for labour and birth. Research has shown that flexibility and fitness can result in a shorter labour, fewer medical interventions and less exhaustion during labour;
- Yoga can help to promote a greater sense of strength, peace and security around the whole birth process; and
- Yoga helps you to breathe deeply which, in turn, helps you to cope with pain.
The benefits of yoga can continue after the birth of your baby, when deep breathing is used to tone the pelvic floor into peak condition and keep your energy levels balanced. Yoga can improve lactation (production of milk supply) and relaxed yoga mothers tend to have relaxed babies.
Yoga classes are held in the Rotunda. The content of the classes includes various breathing techniques, postures and movements followed by deep relaxation. Yoga may help to make you feel calm and help you to deal with whatever challenges lie ahead. The breathing techniques and relaxation are very beneficial for mothers coping with contractions during labour.
Most healthy women can join the yoga classes. Minor disorders of pregnancy generally do not pose a problem. No previous experience of yoga is necessary and you join the classes by phoning up yourself or by getting a letter from your doctor or midwife. The classes are provided by a midwife, are held in the evenings and last about 1 hour 15 minutes to 1 hour 30 minutes. The classes run for six weeks and there is an associated cost. Courses can be repeated.
To make an appointment phone 01 817 6883, between 8.30 am and 4.00 pm, Monday to Friday. If there is no reply, please leave a message with your name and phone number and your call will be returned as soon as possible.
THINGS TO AVOID DURING PREGNANCY
1. Alcohol
The effects of alcohol on a person can vary from person to person. Any alcohol going into a pregnant woman’s bloodstream also goes into her baby’s system. Research shows that when you are thinking of getting pregnant, during your pregnancy and while you are breastfeeding, the best advice is “no alcohol leads to no risk”. Therefore, we recommend that you should not drink any alcohol during this time.
2. Smoking
If you smoke and you are trying to get pregnant or you are pregnant already, you should try to give up. Smoking during pregnancy can seriously affect both your own health and your baby’s development. If you smoke when pregnant you have an increased risk of miscarriage and a higher risk of the placenta coming away from your womb before the baby is born, which can cause premature birth or stillbirth. Babies born to women who smoke have a lower birth weight and more of these babies die from cot death. The sooner you stop smoking the better and it is never too late. Even stopping in the last few weeks of pregnancy can still benefit you and your baby. There are lots of groups and organisations that can help support you to stop smoking.
3. Medications and other drugs
Some medicines, including painkillers, can harm your baby’s health.
As a general rule you should:
- assume that all medicines are dangerous until a doctor or pharmacist can tell you they are safe;
- make sure your doctor or dentist knows you are pregnant before they prescribe anything or give you any treatment; and
- if you take regular medication speak to your doctor once you find out you are pregnant.
However, remember that it is far safer to take many medicines, for example, if you have epilepsy, HIV or diabetes, than to leave the illness untreated.
All illegal drugs, such as heroin, cannabis and cocaine, are dangerous for a pregnant woman. For your own health and the health of your baby, you should not take these from the time you first plan to become pregnant or learn that you are pregnant. For a pregnant woman, there are more risks linked to illegal drug taking. Firstly, drugs may harm your own health, and can affect your ability to support the pregnancy. Secondly, some drugs can directly affect the development of your baby in the womb.
These drugs go through the placenta and reach the baby. The baby becomes addicted along with the mother. At birth, the baby is still dependent on the drug. Because the baby is no longer getting the drug after birth, they can have symptoms of withdrawal such as tremors, sleeplessness, muscle spasms, and sucking difficulties. You can prevent this condition by not taking any drugs during your pregnancy. Talk about all drug use with your midwife and doctor as we can offer additional support to women with drug addiction.
WORK AND TRAVEL
8.1 Coping at work
You may get very tired, particularly in the first and last weeks of your pregnancy. Try to use your lunch break to eat and rest. If you work with chemicals, lead or x-rays, or you are in a job with a lot of lifting, you may be risking your health and the health of your baby. If you have any specific concerns, please talk about them with your doctor, midwife or employer.
8.2 Travel by air
Some airline companies ask for a letter from your doctor or healthcare staff to say that it is safe for you to travel. Research shows that if you travel by air during your pregnancy it can increase the risk of you developing a blood clot. If you do travel it is important to drink lots of water during the flight so that you do not become dehydrated. You should wear ‘flight socks’ and it is important to keep active during a long flight.
8.3 Car safety
Road accidents are one of the most common causes of injury in pregnant women. To protect both you and your unborn baby, always wear a seatbelt with the diagonal strap across your body between your breasts and the lap belt over your upper thighs. The strap should lie above and below your bump, not over it.