Most women will experience some pain after giving birth. It is very important that your pain is well controlled so you can look after yourself and your new baby.
During your time in the Rotunda you will be offered regular pain relief. Pain will be better managed if you take the prescribed medication at regular intervals, rather than waiting until the pain is bad.
Pain relief medications work in different ways and one pain medicine alone may not be enough to control your pain. Depending on your level of discomfort you may be offered two or more medications to control your pain. Combining different types of pain relieving medications may give you better pain control and allows lower doses to be used.
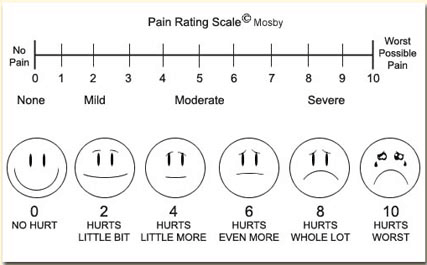
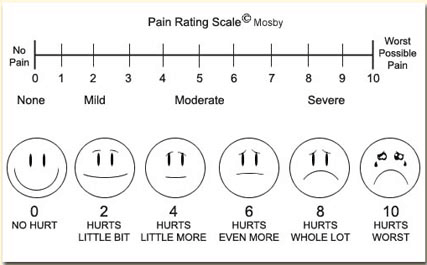
To assess your pain, you will be asked to score it from 0 to 10 where 0 is ‘no pain’ and 10 is ‘worst pain you can imagine’. This will help us to decide which pain medication is best for you, and how much you need. If your pain is not well controlled, please discuss this with your doctor or midwife.
Most women will experience some pain after giving birth. It is very important that your pain is well controlled so you can look after yourself and your new baby.
During your time in the Rotunda you will be offered regular pain relief. Pain will be better managed if you take the prescribed medication at regular intervals, rather than waiting until the pain is bad.
Pain relief medications work in different ways and one pain medicine alone may not be enough to control your pain. Depending on your level of discomfort you may be offered two or more medications to control your pain. Combining different types of pain relieving medications may give you better pain control and allows lower doses to be used.
To assess your pain, you will be asked to score it from 0 to 10 where 0 is ‘no pain’ and 10 is ‘worst pain you can imagine’. This will help us to decide which pain medication is best for you, and how much you need. If your pain is not well controlled, please discuss this with your doctor or midwife.
The following types of pain medication work in different ways and are safe to take together:
– Paracetamol is a very effective pain medication which also reduces fever (high temperature) and inflammation.
– Anti-inflammatories including Ibuprofen or Diclofenac will help reduce levels of chemicals in your body that cause inflammation and pain.
– Opioids such as Oxycodone, Morphine or Codeine are only used if your pain is not well controlled with a combination of other drugs.
Paracetamol
Paracetamol is a very effective pain medication if it is taken at regular intervals. The adult dose is 1gram (two 500mg tablets) four times a day (maximum dose per day is 4grams or eight tablets). If you are taking other medications for pain or over the counter cold and flu remedies, always check with you doctor, midwife or pharmacist if these contain Paracetamol. You should only take one Paracetamol containing product at a time.
Ibuprofen
This can be safely taken with Paracetamol. The usual dose is 400mgs three times a day. Because these tablets can upset your stomach they need to be taken with or soon after food. If you have asthma, Ibuprofen may make it worse. Tell your doctor, midwife or pharmacist if you have asthma or if you are on any other medications as they may interact with Ibuprofen.
Diclofenac
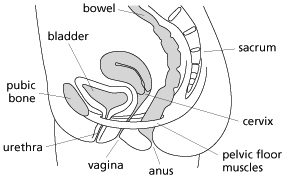
Diclofenac is usually given as a suppository (100mgs once a day). It provides good control of your pain in the days after vaginal delivery or caesarean section. After the first two days you will usually be given Ibuprofen tablets which act in a similar way to Diclofenac. If you have asthma, Diclofenac may make it worse. Tell your doctor, midwife or pharmacist if you have asthma or if you are on any other medications as they may interact with Diclofenac.
Never take Ibuprofen and Diclofenac together.
Opioids
If the above medications do not fully control your pain, stronger Opioid medications will be used. Opioids provide very good pain relief, but they are not used as first-line pain-relievers due to side effects including nausea, vomiting, itch, confusion or dizziness, sweating and constipation.
As opioids may affect your co-ordination or cause drowsiness, you should be careful handling your baby. If you feel very drowsy or short of breath after taking opioids, contact your midwife immediately. You may have to take laxatives while taking opioids to avoid constipation.