Care on the Postnatal Ward For Mother
Pain Relief Following Birth
Most women will experience some pain after giving birth. It is very important that your pain is well controlled so you can look after yourself and your new baby.
During your time in the Rotunda you will be offered regular pain relief. Pain will be better managed if you take the prescribed medication at regular intervals, rather than waiting until the pain is bad.
Pain relief medications work in different ways and one pain medicine alone may not be enough to control your pain. Depending on your level of discomfort you may be offered two or more medications to control your pain. Combining different types of pain relieving medications may give you better pain control and allows lower doses to be used.
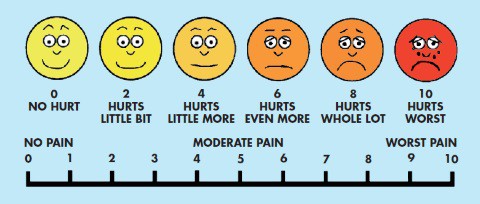
To assess your pain, you will be asked to score it from 0 to 10 where 0 is ‘no pain’ and 10 is ‘worst pain you can imagine’. This will help us to decide which pain medication is best for you, and how much you need. If your pain is not well controlled, please discuss this with your doctor or midwife.
Pain Relief Medications
The following types of pain medication work in different ways and are safe to take together:
- Paracetamol is a very effective pain medication which also reduces fever (high temperature) and inflammation.
- Anti-inflammatories including Ibuprofen or Diclofenac will help reduce levels of chemicals in your body that cause inflammation and pain.
- Opioids such as Oxycodone, Morphine or Codeine are only used if your pain is not well controlled with a combination of other drugs.
Paracetamol
Paracetamol is a very effective pain medication if it is taken at regular intervals. The adult dose is 1gram (two 500mg tablets) four times a day (maximum dose per day is 4grams or eight tablets). If you are taking other medications for pain or over the counter cold and flu remedies, always check with you doctor, midwife or pharmacist if these contain Paracetamol. You should only take one Paracetamol containing product at the time.
Ibuprofen
This can be safely taken with Paracetamol. The usual dose is 400mgs three times a day. Because these tablets can upset your stomach they need to be taken with or soon after food. If you have asthma, Ibuprofen may make it worse. Tell your doctor, midwife or pharmacist if you have asthma or if you are on any other medications as they may interact with Ibuprofen.
Diclofenac
Diclofenac is usually given as a suppository (100mgs once a day). It provides good control of your pain in the days after vaginal delivery or caesarean section. After the first two days you will usually be given Ibuprofen tablets which act in a similar way to Diclofenac. If you have asthma, Diclofenac may make it worse. Tell your doctor, midwife or pharmacist if you have asthma or if you are on any other medications as they may interact with Diclofenac. Never take Ibuprofen and Diclofenac together.
Opioids
If the above medications do not fully control your pain, Opioids may be used. Opioids provide very good pain relief, but they are not used routinely due to side effects including nausea, vomiting, itch, confusion or dizziness, sweating and constipation.
As Opioids may affect your co-ordination or cause drowsiness, you should be careful handling your baby. If you feel very drowsy or short of breath after taking opioids, contact your midwife immediately. You may have to take laxatives while taking opioids to avoid constipation.
Pain relief after leaving hospital
On discharge you will either be advised to buy your medications without prescription in your local pharmacy or you will be given a prescription for pain medications. Bear in mind that pain is much harder to control if you let it build up so please take your medications regularly as recommended at discharge. Further information for those medications will be available on the patient information leaflet inside the pack or from your pharmacist.
Pain relief medications and breastfeeding
Paracetamol, Ibuprofen and Diclofenac are safe for use during breastfeeding. Pain relief medications that contain Codeine or Oxycodone are not used routinely in the hospital if you are breastfeeding. If you are prescribed these medications and you are breastfeeding you need to tell the midwife or doctor if your baby is difficult to wake, does not feed well, does not gain weight, or appears limp or floppy.
After an Epidural
If you had an epidural during your labour and birth, you will need to stay in bed for at least four to six hours after the birth. This allows the effects of the drugs used in the epidural to wear off completely. Do NOT try to get out of bed by yourself. Even if you think your legs feel normal you may become weak when you stand up. You will be given a call bell so please call us for assistance the first time you want to get out of bed.
Lochia
After the birth of your baby you will lose blood from your vagina. This bleeding is normal and is called ‘lochia’. The lochia can be heavy for a few days but will gradually settle down and usually stops within four to six weeks after the birth. The blood loss is caused by your womb contracting as it returns to the way it was before you were pregnant.
If the bleeding gets very heavy (for example, it soaks a sanitary pad in an hour or less) or if you notice any clots or a bad smell from your lochia please tell the midwife looking after you. This could be the start of an infection or a sign of ‘retained tissue’, which could need treatment.
Breast changes
You will experience breast changes in the days after the birth of your baby whether you are breastfeeding or not. This happens as nature prepares to fill your breasts with milk. You will notice your breasts become swollen, hard and sometimes sore. However, this period is short because once you have established breastfeeding your body will regulate the milk supply. If you are not breastfeeding you can help reduce the engorgement by wearing a well-fitting bra with the straps pulled up tightly. It will also help if you avoid stimulating your breasts so don’t put hot water directly on them while in the shower or bath. Breast engorgement will go after a few days if your baby does not stimulate them by sucking to produce milk.
Care of the perineum
Your perineum is the area between your vagina and back passage. If your baby was born vaginally, you may have stitches that become tighter as the wound begins to heal. This can make sitting down, walking and passing urine uncomfortable. Take regular pain relief. You could also try sitting on a cushion to relieve the discomfort.
Wash the perineal area frequently as this will keep the wound clean. Remember to dry yourself well after washing. There is no need to add any disinfectant or salt to the bath water as research has found bathing in plain water is much better for the healing process. It is also important to change your sanitary towels frequently. Do not use tampons as they can cause infection in the early days and weeks after you give birth.
Even if you did not need any stitches after the birth, you may still experience discomfort and heaviness in your vaginal area. This is normal as you are likely to be bruised and swollen around the vagina. Plenty of rest, warm baths, good hygiene and pelvic floor exercises will all help to heal the area.
Passing urine
Emptying your bladder completely after giving birth is very important. You will be asked to measure how much urine you pass when you go to the toilet for the first couple of times after birth. This is so that we know that you are emptying your bladder completely. You should drink at least two litres of fluid a day.
Bowel movements
Many women worry about opening their bowels for the first time after the birth. They are scared that their stitches might burst. Rest assured that this will not happen and in fact the sooner you start going to the toilet the better. If you put this off you may become constipated. To prevent this happening, drink plenty of water and eat high fibre foods such as fruit and vegetables. Gentle exercise will also benefit you.
Blood tests
If your blood group is rhesus negative you may need an injection called Anti-D. We will give you this injection within 72 hours of your baby being born.
During your pregnancy your blood will be tested to see if you are immune to rubella (German measles). If you were not immune to rubella, we can give you the vaccine on the day you are going home. Otherwise, you can get it from your own GP.
If you are rhesus negative and need Anti-D, you should not get the rubella vaccine for a number of weeks. This is because you cannot get these two injections at the same time.
Care following caesarean section
Immediately after surgery
Once your baby is born and providing you and your baby are both well, the baby can be placed directly on your chest for skin to skin contact. Your partner can hold your baby skin to skin if you are unable to do so at the time of birth. Skin to skin contact with you can be continued or commenced on the postnatal ward.
When you arrive on the postnatal ward after your caesarean section, you will have a drip in your arm, through which you will be getting intravenous fluids. You will have a catheter which will drain urine from your bladder for the first 24 hours and you will pass urine normally within six hours of the catheter being removed. There will be a wound dressing on your abdomen over the caesarean section scar, which will be removed after 72 hours. The drip will be continued until you are able to drink enough fluids to stay hydrated and we are sure that the bleeding is not excessive.
If you had a spinal or epidural you will feel numb from the waist down for up to six hours after surgery. After that time, feeling and sensation will gradually come back into your legs. It is important that you do not try to get out of bed on your own during this time. If you had a general anaesthetic, you may feel groggy and sleepy for the first few hours. You may have a special pump attached to the drip through which you receive pain medication. This is known as patient controlled analgesia and the midwife will show you how to regulate the pump yourself.
During the first few hours after surgery, the midwife will be checking your observations regularly, including your temperature, pulse, blood pressure, respiratory rate and oxygen saturations, the wound dressing for signs of bleeding and your vaginal blood loss. She will encourage you to move your body a little in the bed at least every two hours so that a pressure sore will not develop. You will continue to wear white surgical stockings while in hospital and you will be encouraged to bend and move your legs to help prevent a blood clot developing in your leg. You will also receive heparin injections to prevent a clot from forming.
Diet after surgery
Once you are fully awake after surgery, you will be offered sips of water. Usually you can have tea/coffee and toast about four hours after surgery. If you are feeling ok after this we can stop the intravenous fluids. You will be offered a ’light diet’ for the next day or so. You will be ready for a full diet when your bowel is working properly again – either by passing wind or having a bowel motion.
The catering staff will offer you a daily menu choice. If you would like something other than what is on the menu please ask the catering officer. Fruit or nuts can be a good snack especially when you are breastfeeding. Drink plenty of water to prevent dehydration and constipation.
Care of your wound
The wound dressing is removed 72 hours after surgery. You can then have a shower and you should pat dry the wound rather than rubbing it. The wound must be kept clean and dry to prevent an infection. The midwife will check your wound every day. You may have dissolvable stitches, or clips or beads, which will be removed after four or five days. Sometimes the doctor may ask us to leave them in place for a day or two longer. Wear panties that come up above your wound, to avoid friction on the wound site. The physiotherapist will visit you after the operation and she will advise you on postnatal exercises.
Caring for your baby
Your baby will stay at your bedside on the postnatal ward, unless your baby needs admission to the neonatal unit. If you are breastfeeding the midwife will help you and show you different positions to hold your baby so that they will not hurt your wound. The staff will help you to become confident in caring for your baby.
Preparing for discharge
You will know the evening before your discharge that you will most likely be going home the following day. Ask your partner to bring in your clothes and the baby’s clothes and car seat for going home. We will try to have you ready for home by 11 am. We will advise you where to go for your six week postnatal check up. Try to feed your baby just before going home as this will help to keep your baby settled while you are travelling and will give you some time to get settled in at home.
It is common to feel tired after the operation, so try to get as much rest as possible at home. Don’t be afraid to accept help from family or friends with caring for your baby. Avoid lifting heavy objects and driving for six to eight weeks after the operation.
The midwife’s check
The midwife caring for you will carry out a daily postnatal check. They will want to know:
- how you are feeling;
- if you are in any pain;
- if you are experiencing any difficulties with the baby;
- how much you are bleeding vaginally (lochia);
- that you are passing urine without too much discomfort.
The doctor’s check
If your baby was born by caesarean section or if you had an instrumental (vacuum or forceps) delivery then a doctor will visit you on the postnatal ward. They will be happy to answer any questions you have about the birth of your baby.
Sometimes, the doctor may advise you to return to the hospital for your six-week check if they think they will need to talk to you or examine you again. Otherwise you should visit your GP around this time.
Baby blues
-
- It is common to feel a little low a few days after your baby is born.
- The ‘baby blues’ describe weepy moments you may have during this time.
- Feeling overcome, emotional and crying for no apparent reason is a very normal response to the massive change that has happened in your life.
- You can feel overjoyed and frightened all at the one time.
- The tears may start for no reason.
Don’t be frightened by this, just go with it and have a good cry.
As long as every day is not a tearful one you will be fine. Having support on ‘baby blues’ days can be invaluable.
A partner, mother or friend who will cuddle the baby while you have a bath and a cry will seem like a godsend to you!
You will be asked to fill out a simple questionnaire called the ‘Edinburgh score’ before leaving the hospital. It will ask you to consider your mood and feelings at the time around the birth of your baby.
This is a simple tool we use to identify mothers who are emotionally distressed. When you leave hospital, we pass on the score you received on the questionnaire to your GP and public health nurse (PHN). If you do have negative feelings, talking about them and planning a recovery programme can help prevent postnatal depression.
Going home with your baby
How long you stay in hospital will depend on the type of delivery you had or if you or your baby had any complications following birth. We recommend that you stay in hospital for at least 24 hours unless you are going home under the care of the community midwifery team (DOMINO and ETH). If you are breastfeeding for the first time and are not living within the community midwives’ area, we recommend that you stay in hospital for 48 hours. While in hospital, try to get as much rest as possible.
| Guide To You Length Of Stay In Hospital After Birth | |
| If you have access to community midwifery services | 6-24 hours |
| If you don’t have access to community midwifery services and your baby was born by vaginal delivery and you are: |
|
| Breastfeeding | 48-72 hours |
| Formula feeding | 24-72 hours |
| If you had a caesarean section | 3-5 days |
Early Transfer Home (ETH) Service
The ETH service is provided by the community midwives who, if all is well, offer women and babies the opportunity to be discharged from hospital within the first 24 hours following birth.
A midwife from the team will then visit you at home for up to a week to provide care, advice and support. The ETH team operates in the local catchment area of the hospital – the north side of Dublin.
The midwives visit the postnatal wards every morning to arrange for suitable women and babies to go home. If you would like to consider ETH, please phone 01 817 6849 or 817 6850. If you are not within the catchment area for the ETH service then your public health nurse (PHN) will visit you within two days of leaving hospital.
