First Antenatal Visit
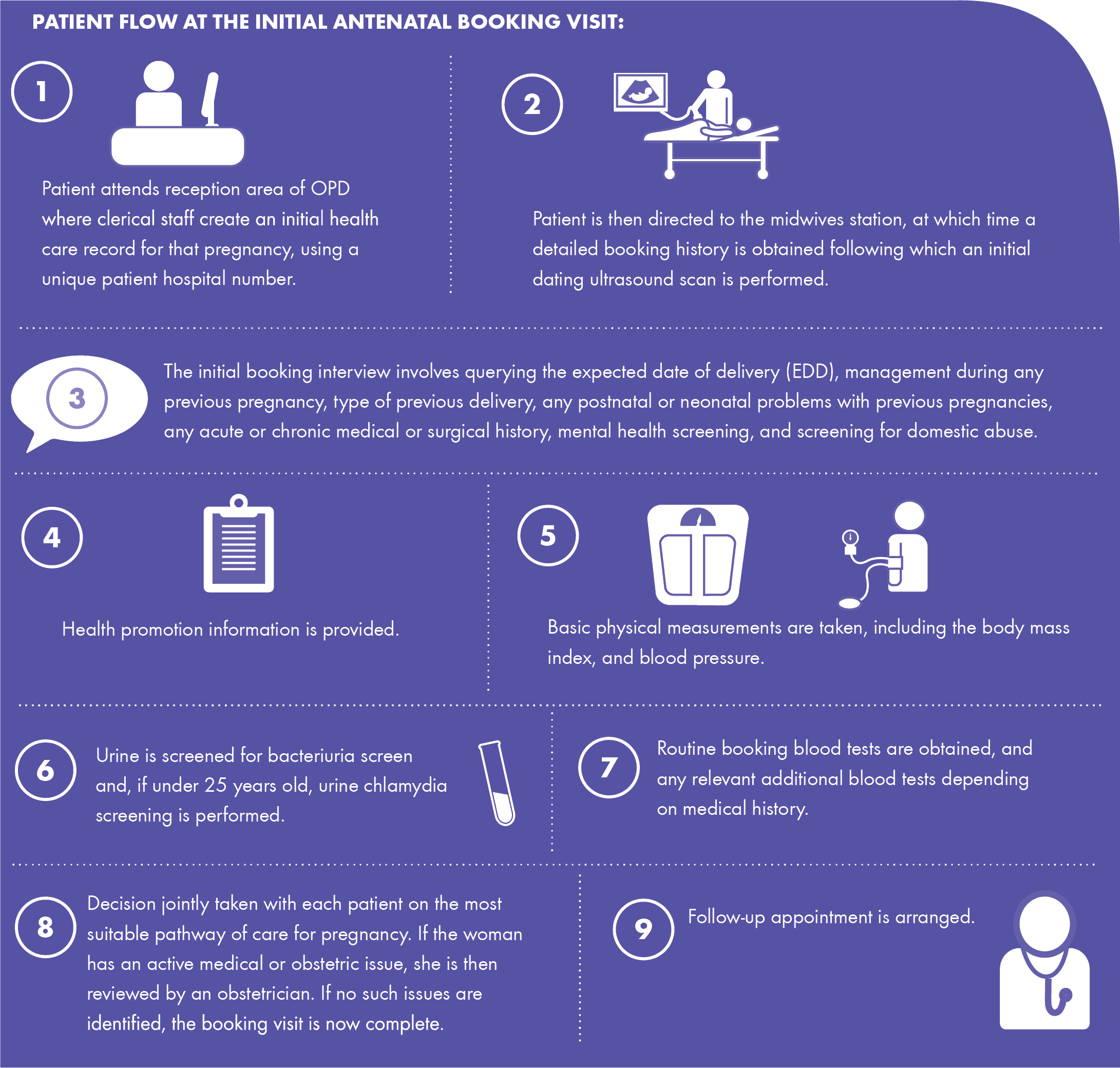
We try to see women who present for a booking visit as quickly as possible. In keeping with best practice guidelines we aim to see women for their booking visit between 12-14 weeks gestation. At this visit you will be seen by a midwife who will take a detailed history and assessment of your medical, surgical, obstetric and psychosocial condition. Following a review of the history, a care plan is chosen to meet your needs. You are seen by a member of the medical team if further consultation is needed, to ensure the most appropriate care pathway for the pregnancy. A baseline recording of blood pressure and a sample of urine (please provide a sample at each visit) will be taken. Blood samples are taken and a dating scan performed by an ultra-sonographer.
The ‘Supported Care Pathway’ is intended for normal risk women and babies. It is delivered by the Hospital and Community Midwifery team and GP.
The ‘Assisted Care Pathway’ is intended for mothers and babies considered medium risk, this care is delivered by Obstetricians and Midwives in the hospital setting and GP.
The ‘Specialised Care Pathway’ for high-risk mothers and babies is led by the Obstetric team and involves midwives as part of a multidisciplinary team. Care will, in the main, be provided in the hospital and may include your G.P.
A woman may need to transfer, either temporarily or permanently between care pathways if an emerging risk is found.
In order to continue to provide the best service we can, we ask two things:
· Please contact us as soon as possible when you know you are pregnant and let us know if you have a particular medical condition
· When attending OPD, please only attend 15 minutes before the SPECIFIC visit time to check-in.
Blood tests
With your written permission, several blood tests are taken. You will be happy to know that all these tests are usually taken at the same time. These blood tests will:
- Check your haemoglobin level (iron), which is the iron containing oxygen in the red blood cells. The baby will take as much of this iron as it needs from your body. This can often leave the mother anaemic and feeling very tired with no energy. The aim is to keep your haemoglobin level above 10.5.
- Check your blood group. There are four types of blood group – A, B, AB or O. For each of the blood groups, there is Rhesus factor – either positive or negative. The rhesus factor is very important in pregnancy because a rhesus negative mother could develop antibodies against the baby’s blood, causing anaemia and jaundice in the baby. For this reason, any woman who has a vaginal bleed or any trauma to her abdomen, such as a blow or a fall, must get their blood group and antibodies checked in the hospital as soon as possible after the event. If rhesus negative, she will be given an injection of Anti-D, which will offer protection to the mother and baby to prevent complications arising in this and future pregnancies.
- Check your rubella immunity (German measles). Women are routinely tested to find out if they have immunity to rubella. Most women are immune to rubella due to the MMR vaccination they received as a child. If the blood test shows that you are not immune, you will be advised how best to avoid exposure to rubella during the pregnancy and you should get the vaccine from your GP after your baby is born.
- Check for sexually transmitted infections. If your blood test is positive for syphilis, you will be offered treatment by means of injections of penicillin. If left untreated, syphilis can lead to miscarriage and stillbirth. Hepatitis B and C are viral infections that can cause liver disease. If you are Hepatitis B positive, giving your baby immunoglobulin treatment soon after birth and follow-up immunisation in the months ahead can protect it. All women are offered testing for HIV and, if you test positive, you will start on antiretroviral treatment, which reduces the risk of transmitting HIV to your baby.
- Check for varicella, which is also called ‘chickenpox’. If you are not immune, you will be advised to avoid direct contact with people who have chickenpox. If you are not immune and you come into direct contact with somebody who has chickenpox, you must contact the hospital, as you may need immunoglobulin to protect your baby.
- Check for sickle cell anaemia and thalassaemia. If you are of African or Mediterranean origin, you will be offered a special test to find out if you have sickle cell or thalassaemia trait. Sickle cell and thalassaemia are inherited blood conditions that affect the way oxygen is carried around the body. Healthy people can be carriers of sickle cell or thalassaemia without knowing it and can pass it on to their children. If you have the trait, your partner will be asked to attend the hospital to check his status, since there is a chance that your baby could develop a double dose of the trait and develop the disease.
The results of all these tests can take up to 14 days to complete. If any test needs to be repeated, you will be contacted by phone or letter by the hospital staff.
You will not receive notification if the blood tests are normal. The results will be filed in your healthcare record for you to see at your next antenatal visit.
Urine Tests
Your urine is checked at every antenatal visit. The two main tests are for protein and glucose (sugar). The most common cause of protein in the urine is an infection in your kidneys or urinary tract. Women are more likely to get infections during pregnancy because all the tubes that make up the urinary system are more relaxed because of pregnancy hormones. Also, the position of the bladder in relation to your womb (uterus) can be a factor. Checking protein levels in late pregnancy is very important, as it can be a sign of the condition called pre-eclampsia.
Glucose in your urine is a concern as it could mean that you are developing pregnancy-related diabetes. If you are found to have glucose in your urine, the midwife will ask you if you were fasting when you gave the sample. If not, she will ask you to return to the hospital the following day with a fasting sample. If this sample is negative for glucose, no action is taken.
If, however, there is still glucose present, the midwife will ask that you have further blood tests to see if you have developed pregnancy-related diabetes. If you have, you will be referred to a specialist team for the remainder of your pregnancy.
Blood Pressure
Checking and recording your blood pressure at the first visit is important.
This first reading is used as a ‘baseline reading’. Every time your blood pressure is checked after that, it is compared to this reading. If your blood pressure rises it could be a sign of pre-eclampsia which needs to be monitored carefully as it could result in the early birth of your baby.
Weight check
If you are of average height and weight, you can expect to gain about 10 – 15 kg (20 – 30 lbs) during the pregnancy. The only time that you are weighed in the hospital is at your first visit. (Women attending the diabetic or anaesthetic clinics will be weighed more often.) It is important not to gain too much weight as this can lead to complications during the pregnancy.
However, it is essential that you eat well and stick to a healthy balanced diet made up of carbohydrates, proteins, fats, vitamins and minerals. Your baby is totally dependent on you for its supply of nourishment in order to grow and develop.
